| |
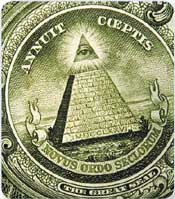 I would like to conclude this session with a photo. For those of you who have a dollar bill in your pocket, this is the Great Seal of the United States that dates back to the 1780s, when the founding fathers were first putting together the United States after the American Revolution. The Great Seal includes two curious mottos, which I’ll share with you, for those of you who were not Latin scholars in school. I would like to conclude this session with a photo. For those of you who have a dollar bill in your pocket, this is the Great Seal of the United States that dates back to the 1780s, when the founding fathers were first putting together the United States after the American Revolution. The Great Seal includes two curious mottos, which I’ll share with you, for those of you who were not Latin scholars in school.
First, Annuit Coeptis, which translates as “Providence has favored our endeavor.” Below that is Novus Ordo Seclorum. This has a number of possible translations but the standard one is, “A new order for the ages.” The historian Paige Smith has given a slightly different translation, which I prefer, “A new age now begins.”
Ladies and gentlemen, I propose this toast to you, Novus Ordo Seclorum.
— George W Sledge Jr, MD
ASCO “Education Session”
May 16, 2005
Orlando, Florida |
The morning after George Sledge sent a stunned ASCO audience into the Orlando sunshine to contemplate six fascinating presentations on monoclonal antibody therapy for breast cancer with trastuzumab and bevacizumab, he met with me to begin the process of making these revolutionary data sets understandable and applicable to physicians in practice. This interview is featured on this program, along with a discussion with the NSABP’s Ed Romond, who presented the combined NCCTG-NSABP adjuvant trastuzumab data at ASCO, and a chat with Jack Cuzick, one of the central figures in the evolution of our other major targeted therapy for breast cancer, endocrine treatment.
When George showed the ASCO multitudes his closing slide of a dollar bill and proposed that “Toto, we’re not in Kansas anymore,” I had the sense that no one in that huge meeting room would disagree with his contention that clinical research in oncology had achieved an unprecedented milestone.
A new age of molecular targeted therapy of cancer has indeed begun, and perhaps the most important take-away from May 16th is that “the system works.” Specifically, it has been possible to:
- Identify a molecular target for an antitumor strategy (HER2 via Dennis Slamon)
- Develop a relatively nontoxic systemic agent to attack that target (trastuzumab)
- Demonstrate that the targeted agent added benefit in the treatment of metastatic disease (Slamon and others)
- Demonstrate robust response rates as monotherapy or with chemotherapy in the neoadjuvant setting (Aman Buzdar, Jenny Chang and others)
- Prove that it substantially reduces relapses and deaths when used as adjuvant therapy (NSABP-B-31, NCCTG-N9831, HERA)
Of equal if not greater importance is that these data once again validate the profound utility of large, well-designed Phase III randomized trials, not only in moving the field forward but also in offering direct benefit to trial participants. This point was made evident during a CME meeting our group hosted in New York immediately after ASCO. An oncologist from Connecticut presented the case of a 35-year-old woman who had initially joined NSABP-B-31 and was randomly assigned to chemotherapy with trastuzumab.
Several weeks later, after researching her options more extensively, the patient decided to drop out of the study because she wished to receive dose-dense AC followed by paclitaxel, which was not part of the NSABP trial design. The patient subsequently developed disease recurrence and is now receiving chemotrastuzumab as palliative treatment for metastatic disease.
While one cannot accurately predict the course of an individual patient, the recent ASCO data suggest that this woman’s statistical likelihood of relapse might have been cut in half had she remained in the study and received trastuzumab.
Like all important clinical research databases, NSABP-B-31, NCCTG-N9831, HERA and ECOG-E2100 have raised as many questions as they have answered, and based on my initial interactions with both clinical investigators and community- based oncologists since ASCO, it is clear that the practical application of these data will be a source of enormous controversy for some time.
Undoubtedly, there will be a sense of urgency to optimize adjuvant trastuzumab algorithms, particularly in patients with pre-existing clinical and subclinial cardiac disease. However, this agent seems to follow the paradigm of other adjuvant therapies, and the classic risk-benefit calculations learned with chemotherapy and endocrine treatment apply to this agent. Peter Ravdin has already begun the process of factoring in the effect of trastuzumab on the very popular website Adjuvant! (www.adjuvantonline.com/online.jsp).
Bevacizumab is another story. While in some ways, the data from E2100 are similar to what was seen when the “other” monoclonal antibody (trastuzumab) was added to chemotherapy in the metastatic setting, bevacizumab does not have an identified target to separate out a patient population for treatment as HER2 does for trastuzumab. This has economic implications, but the situation with bevacizumab goes beyond dollars.
The E2100 data arrive at a time when there has been widespread support among clinical investigators for a minimalist approach to chemotherapy for metastatic breast cancer. Much of this is the result of ECOG-E1193, for which George was the principal investigator. This classic study revealed that while combination chemotherapy improved response rate and short-term tumor control, longterm survival was the same as with sequential single agents. These data were often cited when subsequent combination chemotherapy trials — for example, Joyce O’Shaughnessy’s US Oncology study evaluating capecitabine/docetaxel — demonstrated improved progression-free survival and overall survival.
E2100 did show an overall survival benefit when bevacizumab was added to paclitaxel, although these data will be more mature and interpretable later this year. However, this study — as with Joyce’s “XT” trial — did not mandate a crossover to the second agent, and this leaves room for controversy. On the other hand, bevacizumab seems to have considerably less adverse impact on quality of life than cytotoxic therapy. So perhaps what seems like some confusion about practical implications of this data set will quickly resolve if future studies demonstrate that in some way, this unique agent is a general potentiator of all cytotoxic regimens. In the future, we may be routinely combining bevacizumab with chemo just as routinely as we now add in anti-emetics. If this happens, there will undoubtedly be even more challenging questions about who will pick up the tab for this considerable investment, although it is clear that most patients desperately value any extension of the time of disease control and their survival, particularly as the result of a relatively nontoxic treatment.
Our group is about to conduct another patterns of care study on randomly selected US-based medical oncologists, and it will be very interesting to see what people are doing about adjuvant and neoadjuvant trastuzumab and bevacizumab for metastatic disease. With regards to the anti-VEGF agent, docs might just end up in the future choosing the exact same first-line chemo regimen they chose before ASCO — and just add bevacizumab. It is also likely that — as with trastuzumab in metastatic disease — there will be considerable discussion about whether to continue bevacizumab and switch chemo agents on disease progression.
In terms of adjuvant trastuzumab, by the grace of whatever or whomever you believe in, one in four or five breast cancer patients will now walk out of their initial consultation with a medical oncologist knowing that on May 16th, their risk of cancer recurrence was further lowered by 50 percent.
Like George says, Annuit Coeptis.
— Neil Love, MD
NLove@ResearchToPractice.net
|
|

