 |
Editor’s Note |
|
| Four very cool dudes |
It’s almost impossible to believe that I actually get paid to chat with people like Mike Baum, Norm Wolmark, Gabe Hortobagyi and Jay Harris. The only job that might be better would be sitting next to John Madden as co-color commentator for Monday Night Football. (“Hey John, let me use that telestrator to show the folks how the HER2 system integrates with AKT!”). The bottom line is that I love my job and the people I meet.
My first exposure to Mike Baum was in the late 1980s when he was raising hell about tamoxifen. Mike loves to push people’s buttons, particularly when he’s right, which is very frequently. At that time, he was quite incensed that many of his colleagues in the research community believed that tam was ineffective in premenopausal patients. These researchers were concerned that women experienced tamoxifen-related serum estradiol spikes; however, Mike’s trials in the United Kingdom suggested the same clinical antitumor benefit as was seen in postmenopausal patients.
It wasn’t until the 1995 International Overview that it became apparent that Mike was right (again), and by then many patients had relapsed or died. Eventually, the lack of benefit in prior Overviews proved to be the statistical result of too few observed events.
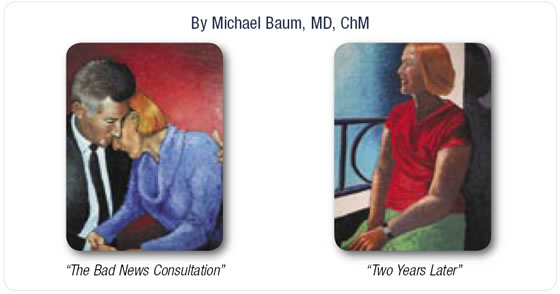
People who don’t know Mike sometimes misinterpret his outspoken nature for egocentricity, but I see him as a champion of the patient, who fights for every possible advantage against a vicious disease. During the most recent interview for this program, he gently chides Norm Wolmark and the NSABP on a variety of issues. I can induce instant apoplexy in Mike by simply raising the subject of screening mammography. (He questions its value in many situations.) But as tough as Mike is, he is also a renaissance physician whose award-winning oil paintings (see page 5) tell a lot about the person inside the investigator.
Norm Wolmark is another unique research leader. His comments always have a whimsical tone, as if to say, “Just because I am the chairperson of the NSABP, doesn’t mean I have every answer.” Norm is a perfect successor to Bernie Fisher; both tell it like it is and don’t much care what anyone else thinks about it.
These legends love to challenge existing paradigms. It is testimony to their leadership that after decades of implementing some of the classic randomized trials that have defined the roles of many standard therapies, these studies are now delivering a second wave of important new data, with the landmark work of pathologist Soon Paik and his crew.
Soon is restudying tissue from patients who participated in past NSABP trials and correlating these findings with outcome. The stunning results were the most discussed presentations at the past two San Antonio Breast Cancer Symposiums. In December 2003, Soon presented the first results of the Genomic Health assay, which was a milestone in tumor prognostics. A year later he presented a second data set that has the potential to immediately and dramatically change the treatment of the largest current subset of newly diagnosed patients with breast cancer — those with node-negative, ER-positive tumors.
Essentially, the Oncotype DX™ assay was able to differentiate between a group of patients who experienced a 75 percent reduction in relapse rate from chemotherapy and a second group that derived no benefit. Not surprisingly, behind all of this is paradigm-shifter Norm, who, in his spare time, also leads the way in colorectal cancer research.
Gabe Hortobagyi — another larger-than-life figure — provided perhaps the single most compelling interview I have conducted in my career. It was 2002 and the initial ATAC trial data had recently been presented. Investigators and community-based clinicians were scrambling to figure out what this fascinating data set meant for patient care. Even Mike Baum — who presented the findings in San Antonio — wasn’t sure whether the data justified substituting anastrozole for arguably the most important antitumor agent in the history of cancer care (tamoxifen).
Gabe saw it very differently, as did his MD Anderson colleague, Aman Buzdar. Both of these highly respected investigators strongly endorsed the use of anastrozole as the preferred initial adjuvant endocrine therapy for postmenopausal women with receptor-positive tumors. During the interview, I explored with Gabe his thinking about this dramatic shift in practice, and he confided in me (and to a national audience) that his rationale for taking action on what many saw as preliminary data was partially based on regret he felt from a prior time.
In an extraordinary conversation, Gabe confessed that for many years he has questioned his own actions as they relate to adjuvant tamoxifen. Specifically, he noted that in the early 1990s, while Mike Baum and others were emphatically stating that tamoxifen was effective in premenopausal patients, he was equally insistent that existing data was inadequate to support treatment.
In fact, MD Anderson’s clinical trials at that point did not include tamoxifen for premenopausal women with hormone receptor-positive disease. Sadly, it is now clear that many women might have been spared recurrence had they received tamoxifen, which has become the standard of care against which other therapies are compared.
It’s easy to say that we have seen instances such as stem cell transplantation, in which the early incorporation of therapies into the treatment algorithm has caused unnecessary morbidity and mortality. But, in balance, Gabe’s philosophy changed fundamentally when he learned from the 1995 Overview data that his judgment was flawed — particularly when considering the relatively modest risk of tamoxifen. When ATAC came along, things were different, and the leadership that Gabe and others provided has accelerated the adoption of anastrozole and other aromatase inhibitors as the standard of care for postmenopausal patients.
I interviewed Gabe and Jay Harris shortly after moderating a tumor-panel discussion in which Gabe surprised the audience with an emphatic statement about the practice of switching from tamoxifen to an aromatase inhibitor. Essentially, he said that when he evaluates a postmenopausal woman who is receiving adjuvant tamoxifen, he switches her to an aromatase inhibitor regardless of how long she has received tamoxifen. This statement provided a simple but controversial answer to a much-debated issue. When I asked Jay about it in our interview, he said, “Everyone respects Gabe enormously, and we have learned over the years that what he says is usually correct and what he predicts is usually where we are heading.”
That brings us to radiation oncologist Jay Harris, who has an encyclopedic knowledge of the disease and, in fact, edits the “encyclopedia of breast cancer” (Breast Diseases, published by Lippincott, Williams & Wilkins). Jay embodies the term “radiation oncologist,” just as Mike Baum and Norm Wolmark are “surgical oncologists.” Oncologists are interested in the disease process and the people who suffer from it. They ruminate together every week in tumor boards about the potential impact of interventions not only on the tumor, but also on the host. Breast cancer patients desperately need these oncologists and also, the four amazingly cool dudes interviewed in this issue of Breast Cancer Update and their investigator colleagues.
So here I am, wide-eyed, fascinated and listening intently as these research giants tell tales and make predictions for the future. It’s fun, interesting, exciting and a pleasure to bring to you.
— Neil Love, MD
NLove@ResearchToPractice.net
|

